Introduction
Crohn’s disease is a chronic inflammatory condition that affects the gastrointestinal (GI) tract. As one of the main types of inflammatory bowel diseases (IBD), Crohn’s disease causes discomfort, disruption of daily life, and, in severe cases, can lead to serious complications. Although there is no definitive cure, understanding the disease and following a tailored treatment plan can greatly improve the quality of life for those affected.
In this comprehensive guide, we’ll explore the root causes, primary symptoms, diagnostic techniques, available treatments, and strategies for managing Crohn’s disease effectively.
What is Crohn’s Disease?
| Aspect | Details |
|---|---|
| Definition | Crohn’s disease is a long-term condition causing inflammation in parts of the digestive tract. |
| Commonly Affected Areas | Primarily impacts the small intestine and colon. |
| Disease Type | A form of inflammatory bowel disease (IBD). |
| Prevalence | Affects millions globally, with increasing rates in developed countries. |
| Typical Age of Onset | Most commonly diagnosed in individuals between 15 and 35 years old. |
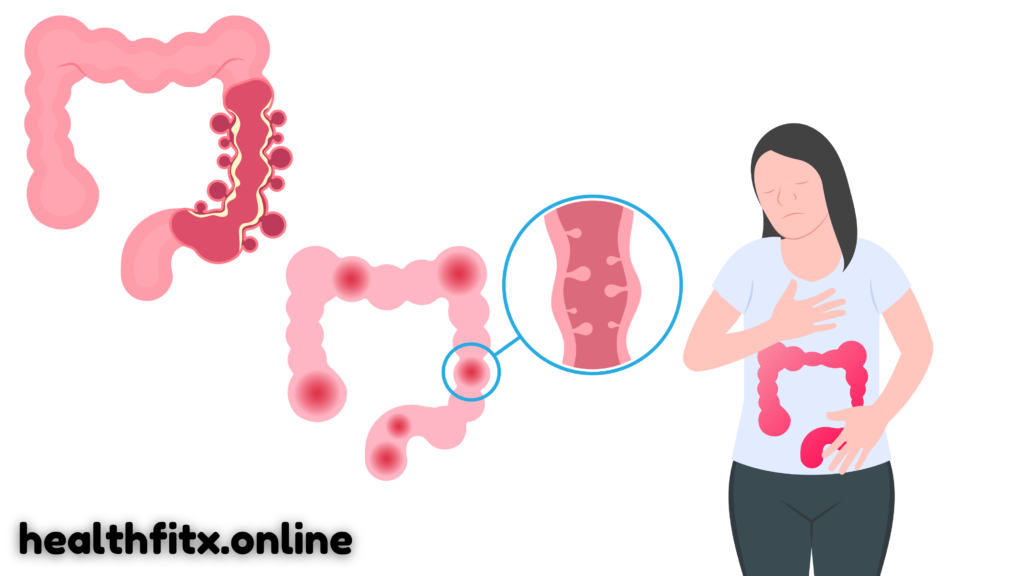
Crohn’s disease is a chronic condition that causes inflammation anywhere along the digestive tract, though it typically impacts the small intestine and colon. This condition falls under the umbrella of inflammatory bowel diseases (IBD), which also includes ulcerative colitis. People with Crohn’s disease experience periods of flare-ups followed by periods of remission.
Despite extensive research, the exact cause remains unclear, but genetics, immune system dysfunction, and environmental factors are believed to play key roles.
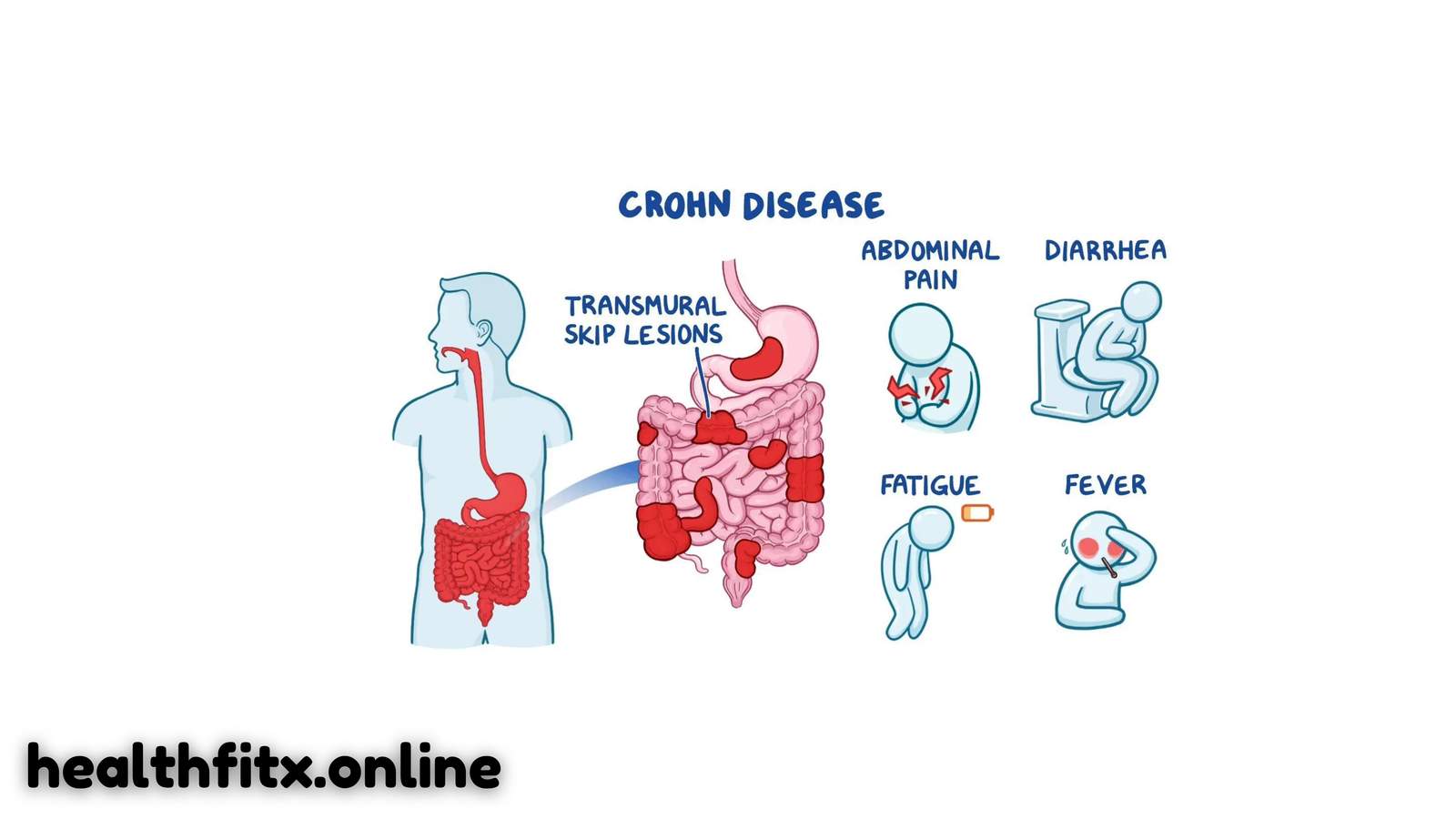
Signs and Symptoms of Crohn’s Disease
| Symptom | Details |
|---|---|
| Abdominal Discomfort | Cramping or persistent pain in the abdomen, often in the lower right side. |
| Chronic Diarrhea | Diarrhea lasting for weeks, sometimes with mucus or blood. |
| Weight Loss | Unexplained weight loss due to poor nutrient absorption. |
| Fatigue | Tiredness that doesn’t improve with rest. |
| Blood in Stool | In some cases, stools may contain visible blood. |
| Fever | Low-grade fever often accompanies active inflammation. |
The symptoms of Crohn’s disease can vary depending on the severity and location of the inflammation. Common symptoms include abdominal pain, diarrhea, and weight loss, while some people also experience fatigue, fever, and blood in their stool. These symptoms may worsen during flare-ups and can make it difficult for individuals to manage daily life.

What Triggers Crohn’s Disease?
| Cause | Details |
|---|---|
| Genetics | Family history of IBD increases the likelihood of developing Crohn’s disease. |
| Immune System Abnormalities | An overactive immune response is believed to contribute to the inflammation seen in Crohn’s disease. |
| Dietary Factors | Certain foods may trigger or exacerbate symptoms, although diet’s role is still being studied. |
| Smoking | Smoking is a known risk factor that can worsen the disease. |
| Age and Ethnicity | Most commonly diagnosed in young adults, with higher prevalence among Ashkenazi Jews. |
Crohn’s disease is thought to result from a complex interaction of genetic and environmental factors. People with a family history of IBD are more likely to develop the disease. Additionally, an overactive immune system, environmental factors like smoking, and diet can influence the disease’s progression. People of Jewish descent—particularly those with Ashkenazi Jewish heritage—have a higher risk of Crohn’s disease.
How is Crohn’s Disease Diagnosed?
| Test | Purpose |
|---|---|
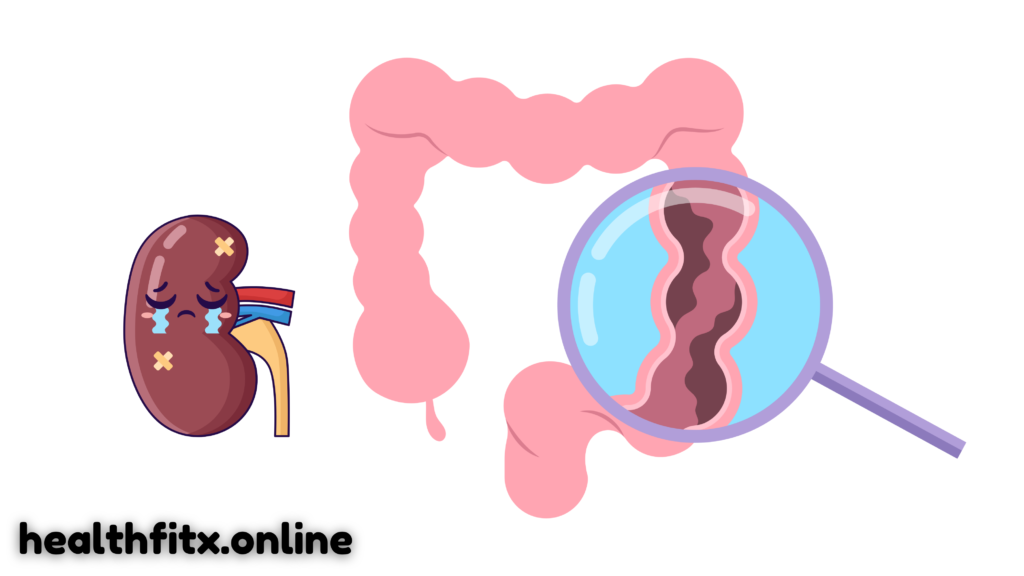
| Endoscopy | A tube with a camera is inserted into the GI tract to view inflammation. |
| Colonoscopy | Examines the colon and rectum to detect inflammation or other abnormalities. |
| Biopsy | A tissue sample is taken to assess the extent of inflammation. |
| Blood Tests | Used to check for signs of infection, anemia, or inflammation. |
| Stool Tests | Ruling out infections or other causes of digestive symptoms. |
Diagnosing Crohn’s disease typically involves a combination of imaging tests, biopsy, and blood work. Colonoscopy is one of the most common diagnostic procedures, which allows doctors to view the inflamed sections of the intestines directly and take biopsies for further testing. Blood tests may show signs of anemia or elevated levels of inflammation, while stool tests are useful in ruling out infections.

Treatment Options for Crohn’s Disease
| Treatment Type | Details |
|---|---|
| Medications | Includes anti-inflammatory drugs, immunosuppressants, and biologics. |
| Dietary Modifications | Certain diets can help reduce symptoms and improve nutrition. |
| Surgical Interventions | Surgery may be necessary in severe cases or when complications arise. |
| Probiotics | Beneficial bacteria that may help restore gut health. |
While Crohn’s disease cannot be cured, it can be effectively managed with a variety of treatment strategies:
Medications:
The first line of treatment includes anti-inflammatory medications such as aminosalicylates. For more severe cases, immunosuppressive drugs and biologic therapies (e.g., TNF inhibitors) may be prescribed. These help suppress the immune response and reduce inflammation in the GI tract.
Diet:
Dietary changes are also important. Many people with Crohn’s disease benefit from a low-fiber diet or specialized eating plans like the Specific Carbohydrate Diet (SCD). Nutritional supplements might be necessary to address nutrient deficiencies, especially if the disease leads to malabsorption of essential vitamins and minerals.
Surgery:
In some cases, surgery becomes necessary if medications are ineffective. This may involve removing sections of the intestines, repairing fistulas, or addressing complications like abscesses.
Managing Crohn’s Disease Effectively
| Management Strategy | Details |
|---|---|
| Ongoing Monitoring | Regular check-ups to assess disease progression and treatment efficacy. |
| Stress Reduction | Methods like yoga, mindfulness, and exercise to reduce flare-ups. |
| Support Systems | Support groups and counseling for emotional and psychological support. |
| Healthy Lifestyle | Avoiding smoking, drinking alcohol in moderation, and maintaining a balanced diet. |
Living with Crohn’s disease involves continuous management and adaptation to the challenges the disease presents. Regular visits to a healthcare provider are essential for monitoring disease activity and adjusting treatment plans. Stress management plays a key role in minimizing flare-ups, as stress is known to worsen symptoms. Lifestyle changes, such as avoiding smoking and eating a balanced diet, can also help maintain long-term health.
Living with Crohn’s Disease: Practical Tips
| Lifestyle Consideration | Tips for Managing Crohn’s Disease |
|---|---|
| Exercise | Engage in gentle exercise like walking, swimming, or yoga to improve overall health. |
| Sleep Hygiene | Prioritize restful sleep to help maintain a strong immune system. |
| Dietary Adjustments | Work with a nutritionist to identify trigger foods and improve gut health. |
Living with Crohn’s disease requires adopting a proactive approach to health and wellness. Regular exercise, adequate sleep, and maintaining a nutritious diet are essential for managing the disease. Some individuals may find that specific foods trigger their symptoms, so keeping a food diary can be a helpful way to pinpoint these triggers.
Recent Research and Future Outlook
| Research Area | Details |
|---|---|
| New Medications | Continued advancements in biologics and other drugs targeting specific immune mechanisms. |
| Gut Microbiome | Exploring the role of gut bacteria in managing IBD and Crohn’s disease. |
| Gene Therapy | Investigating genetic interventions to alter immune responses to prevent inflammation. |
Recent advances in medical research offer hope for improving treatments for Crohn’s disease. Biologic therapies are becoming more targeted and effective, reducing symptoms and preventing flare-ups. Additionally, understanding the role of the gut microbiome in disease progression could open doors to more personalized treatments in the future.
Conclusion
Although **Crohn’s
disease** is a chronic and challenging condition, advancements in medical treatments, lifestyle management, and ongoing research provide hope for those affected. While there is no cure, adopting a comprehensive approach—combining medical treatment with dietary and lifestyle changes—can significantly improve quality of life. With continued research into the causes, treatments, and management of Crohn’s disease, there is optimism for better outcomes in the future.
For anyone diagnosed with Crohn’s disease, it’s crucial to stay informed and work closely with a healthcare provider to create a tailored treatment and management plan that fits their unique needs.